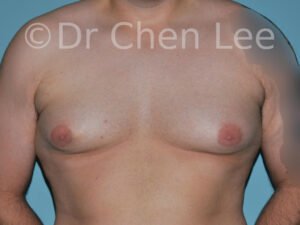
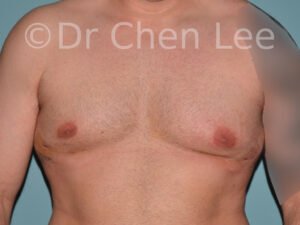
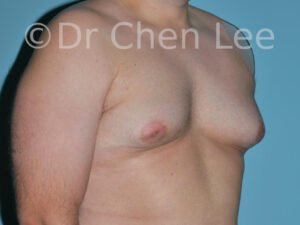
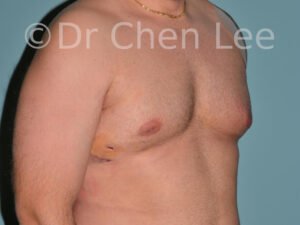
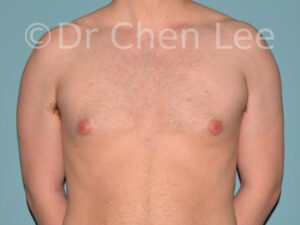
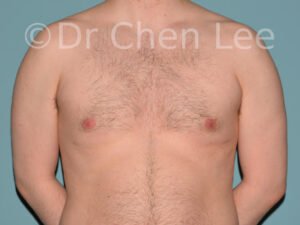
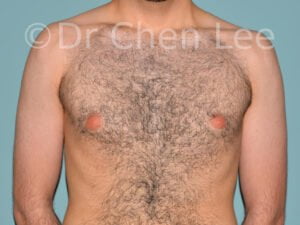
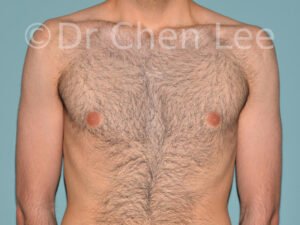
Gynecomastia
Male breast enlargement can be socially devastating. Gynecomastia surgery can greatly change your life.
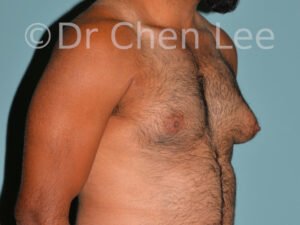
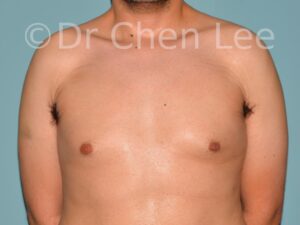
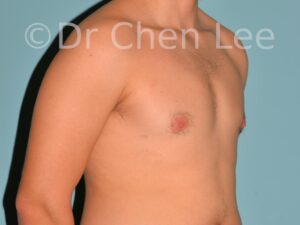
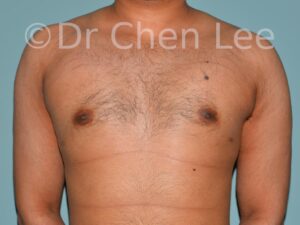
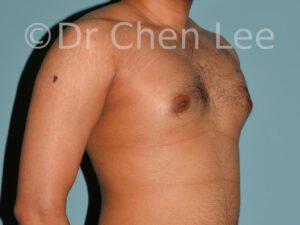
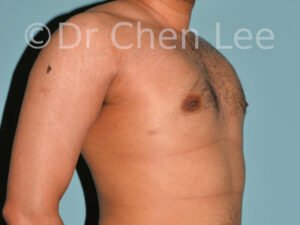
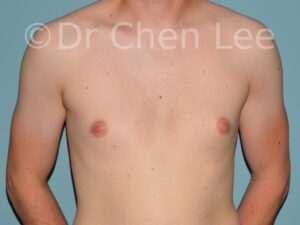
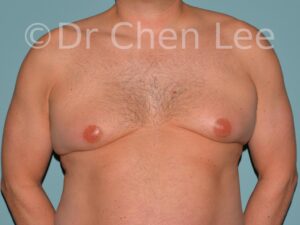
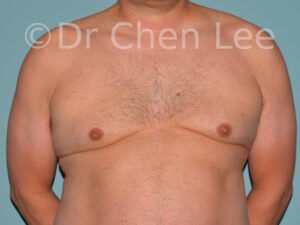
Gynecomastia is commonly referred to as “man boobs” and “gyno”. Estimates of up to 20% of adolescent males are affected by this medical condition. In this condition, breast tissue develops and can enlarge into a significant mammary shape that has a feminine form. Affected men often have doming of the areola giving a “puffy nipple” appearance to the nipple-areola complex of the breasts. In most cases, the breast tissue is entirely normal and does not pose a risk to the affected individual’s physical health. However, the psychosocial impact necessitates this condition to be taken seriously. Unfortunately, many misconceptions and unproven nonsurgical treatments are promoted. Gynecomastia surgery has been a proven and effective method of masculinizing the chest.
Gynecomastia – The Essentials
During your consultation, we’ll help you to feel comfortable explaining your goals and expectations.
Gynecomastia Considerations
Gynecomastia is also known as “man boobs” & “gyno”, occurs when a feminine contoured breast develops in a man. It affects up to 20% of adolescent males.
All humans are born with hormonally sensitive mammary tissue. During puberty, a rise in estrogen naturally occurs in women. This stimulates the mammary tissue to develop into a breast form associated with feminity. During a woman’s life, many factors (pregnancy, age, disease) will affect the breast size, shape, symmetry, nipple, and areolar dimensions.
Similarly, mammary tissue in males will also undergo changes during puberty. In general, estrogen levels are lower in males and breast development usually does not exceed beyond the pigmented skin of the areola surrounding the nipple. For unknown reasons, some men have continued growth of their mammary tissue into feminine-shaped breasts.
If you are a man, the progressive development of a feminine breast is one of the most common and distressing life events. Usually, there is no identifiable cause. This is medically known as developmental gynecomastia. Special medical investigations are not necessary with this type of gynecomastia.
Breast development in preadolescent children is abnormal and should be medically investigated. Diseases of the pituitary gland or testes may cause prepubescent breast development. Similarly, adult men who develop gynecomastia should be evaluated for recreational drug use (marijuana), medications, illness, or endocrine dysfunction. When one breast enlarges in an adult man, an urgent and thorough evaluation to rule out male breast cancer is warranted.
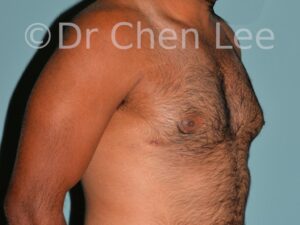
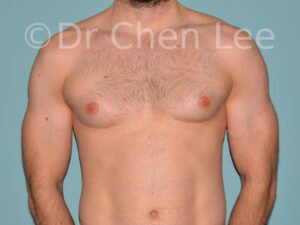
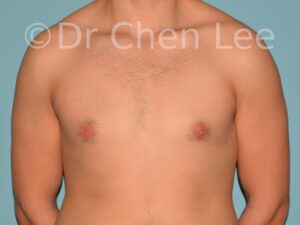
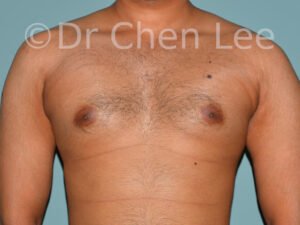
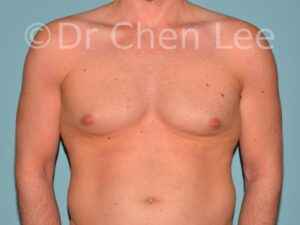
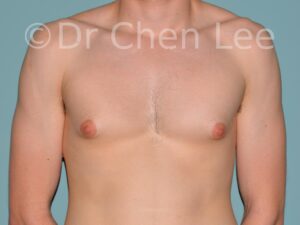
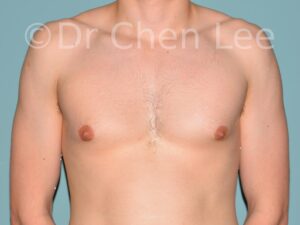
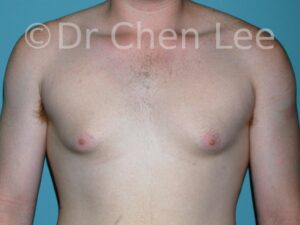
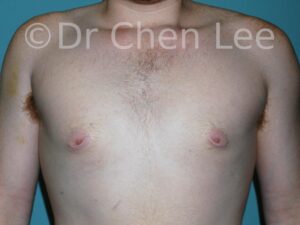
Fortunately, developmental gynecomastia is well managed with male breast reduction. Dr. Chen Lee understands that gynecomastia surgery requires attention to detail. To yield the best possible cosmetic outcome, he will formulate a surgical plan based on your unique breast anatomy.
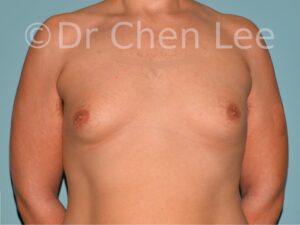
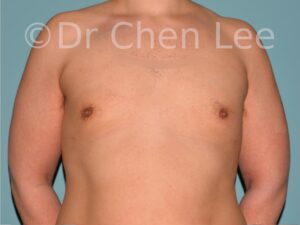
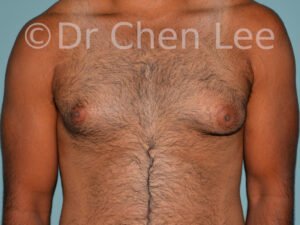
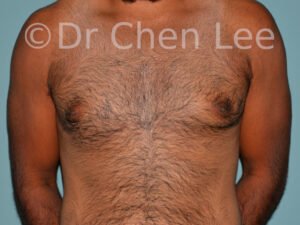
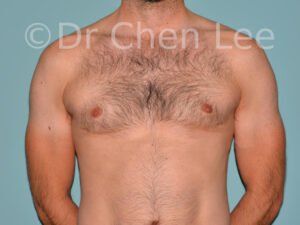
The spectrum of gynecomastia severity has been categorized into a grading system:
- Grade I: Minor enlargement, no skin excess
- Grade II: Moderate enlargement, no skin excess
- Grade III: Moderate enlargement, skin excess
- Grade IV: Marked enlargement, skin excess
Nonsurgical treatments such as exercise to build the pectoral muscles, special diets, and skin creams do not work. If a medical reason for the gynecomastia is identified, then treatment of the underlying health problem may be sufficient to treat the gynecomastia. However, the vast majority of adult men affected with gynecomastia will require surgery.
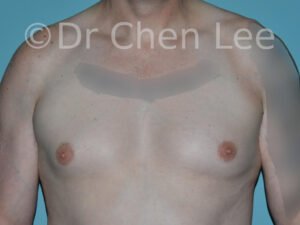
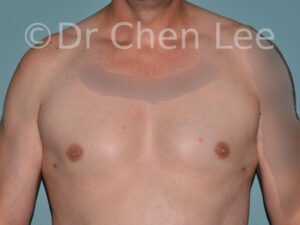
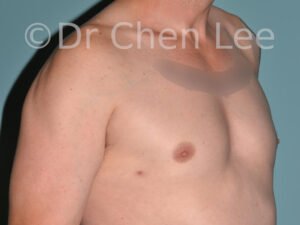
Male breast reduction can consist of liposuction to remove breast fat, direct excision of the gland, and/or skin excision.
Liposuction is especially effective when the skin envelope is normal and the gynecomastia is comprised primarily of fatty tissue. A bulging fatty feminine breast can be sculpted into a pleasing masculine contour aspirating the fat using tiny skin incisions. Liposuction is ineffective for a “glandular” breast.
Direct excision techniques are necessary when the breast is comprised of firm glandular tissue. Strategically positioned incisions around the areola or inframammary fold are commonly used when performing direct glandular excision of a gynecomastia enlarged male breast.
Skin reduction and nipple grafts are sometimes necessary to manage the excess skin associated with gynecomastia grades 3 and 4. To achieve a masculine chest contour, the skin excisions used with these severe cases of gynecomastia will result in a loss of nipple sensation, and leave visible scars around the areola and at the inframammary crease.
The plastic surgery techniques used to treat gynecomastia are varied. Optimal outcomes are best achieved when the surgical plan is designed to address your unique anatomy. Dr. Chen Lee will customize a male breast reduction (liposuction of fat, direct glandular excisions, skin reductions) to masculinize your chest.
Gynecomastia Surgery

Our plastic surgeon, Dr. Chen Lee, will perform a thorough examination to determine the ideal gynecomastia procedure for your unique situation. A written detailed list of risks and complications will be provided. We encourage you to read it.
If your procedure is planned under general anesthesia, we will order routine laboratory tests to evaluate your fitness for male breast reduction.
Below are some basic recommendations to prepare for gynecomastia surgery:
- 1 month prior to surgery stop use of any tobacco or substances containing nicotine and do not resume until healed (usually 1 month after surgery)
- 1 month prior to surgery stop use of all street drugs
- 2 weeks before surgery avoid the use of nonsteroidal anti-inflammatory medications (eg. Aspirin, Advil, Motrin, etc.)
- on the evening and morning before surgery, shower with an acne soap such as Spectro-Jel
- if your procedure is planned under general anesthesia, it is important to fast (not eat or drink anything) after midnight before surgery
Dr. Chen Lee’s gynecomastia patients are usually managed as ambulatory day surgery patients.
Minor male breast reductions performed under local anesthesia are usually scheduled as the final case during the afternoon of a routine workday. These local anesthesia procedures typically are short requiring 1 to 2 hours of your day.
More extensive gynecomastia procedures under general anesthesia require greater planning and attention to details. Our patients should plan for the following when their male breast reduction is scheduled under general anesthesia:
- Plan to be occupied at the surgical center for half a day.
- Arrive at the surgical center at the requested time.
- Our nursing team will greet and prepare you for safe surgery.
- To have a safe general anesthetic, you must arrive at the surgical center in a fasted state (i.e. nothing by mouth 8 hours before surgery).
Male breast reduction performed under general anesthesia typically requires 2:00 to 3:00 of operative time.
- When you wake up, you will be taken to a recovery room.
- Once the anesthetic has worn off, you will be transferred to an observation unit for 1-2 hours before discharge home.
Your safety is our utmost concern.
- You must be accompanied home by a trusted friend or family member.
- We recommend that they be present in your home for the early days following rhinoplasty.
Our office will call by telephone to periodically check on your progress at home. If you have a breast drain, our nurses will instruct you on how to empty and record the output. It will be removed at the first office visit 5-10 days after surgery.
Our gynecomastia patients usually do not require a drain following male breast reduction. If a breast drain is placed by your surgeon, instructions as to emptying and recording the output will be provided prior to your discharge from the surgical center.
You will be provided a compressive garment or vest to wear for 2 to 6 weeks. The compressive garment must be frequently adjusted to ensure it is comfortably snug. It is easily hidden under loose clothing and can be removed to shower.
Patients having local anesthesia for minor gynecomastia surgery can often return to their usual routines without disruption. For moderate male breast reduction performed under general anesthesia, we advise a 1-week cessation of work. Return to sports and intense physical activities is usually possible after 3 weeks.
Complications following gynecomastia surgery are infrequent.
Bleeding, infection, hematoma, and seroma are possible. If severe, go straight to the hospital emergency room hospital without delay.
Delayed wound healing and skin necrosis are complications that occur more often in obese patients and smokers. Wound complications are associated with increased scars.
Incisional scars are short and not easily seen. Additionally, the scars fade with time (>6 months) and are easy to conceal with clothing. Occasionally, scar revision is necessary. Surgical revisions are usually minor procedures performed under local anesthesia.
Early after surgery, most patients experience a loss of sensation in the nipple and areola. This will spontaneously improve after 6 months.
During your consultation, Dr. Chen Lee will answer your questions and address concerns about complications. Our office will also provide you with a more comprehensive document listing the risks and complications associated with gynecomastia surgery.
Gynecomastia Surgery Costs

The initial office consultation for gynecomastia surgery is a wonderful opportunity to establish a healthy patient-surgeon relationship. During the consultation, the plastic surgeon will typically perform a breast exam, recommend a technique specific to your case, discuss the possible incisions, and the expected outcome following male breast reduction. In addition, the risks associated with gynecomastia surgery will be explained and given in writing. For the patient, he should use this initial encounter to judge the professionalism and qualification of the doctor, as well as the quality of the information transmitted. With a comprehensive understanding of your goals, the plastic surgeon will be better able to achieve your objectives and make your gynecomastia safe and satisfying.
The price of male breast reduction in Montreal is quoted as a “global fee”. The price quote includes the costs of the surgeon, anesthesiologist, nurses, office visits during the first postoperative year, operating room, and surgical facility fees. Revisions and touch-up surgeries are not included in the initial gynecomastia surgery quotation. If general anesthesia is necessary, you will have to pay for the substantial costs associated with a surgical revision. Minor touch-up surgery under local anesthesia can often be performed at minimal expense.
Gynecomastia surgery pricing is proportional to its complexity. The prices below are for the treatment of both breasts. When male breast reduction is required in only one breast the price is adjusted lower.
Mild gynecomastia often can be treated with glandular excision under local anesthesia. The price range for minor male breast reduction under local anesthesia is $4,000 – $6,000 +taxes.
Moderate gynecomastia not requiring skin reduction generally responds well to a combination of liposuction and gland excision performed under general anesthesia. The price range for moderate male breast reduction under general anesthesia is $9,000 – $10,500 + taxes. This is the most commonly quoted price for patients seeking gynecomastia surgery in Montreal.
Complex gynecomastia surgery often involves skin reduction in addition to liposuction and gland excision. The price range for complex male breast reduction under general anesthesia is $10,500 – $15,000 + taxes.
Our office requests payment in 2 equal installments. To reserve a date at the surgery center, we request an accompanying first installment (50% payment). The remaining balance is due 3 weeks before your scheduled date of surgery.
Surgeries are payable in cash, certified checks (bank drafts), or Interac. We also work with and an independent credit company that offers financial payment plans for cosmetic surgery procedures. However, you should be aware that the interest rates and administration fees of this specialized company are higher than traditional financial institutions. It is often better to negotiate a loan through your personal bank or financial institution. We encourage you to do your homework and compare the true financial cost of these various financial options.
Gynecomastia surgery is performed either under local or general anesthesia on ambulatory patients as an outpatient procedure. Most patients experience mild discomfort and swelling of the chest.
We tailor our aftercare recommendation to every patient’s unique situation. Post-operative care generally consists of wearing a compressive garment for 2 to 6 weeks and avoidance of intense physical activities. The compressive garment is easily hidden under loose clothing. Patients having local anesthesia for minor gynecomastia surgery can often return to their usual routines without disruption. For moderate male breast reduction performed under general anesthesia, we advise a 1-week cessation of work. Return to sports and intense physical activities is usually possible after 3 weeks.
FAQ – GYNECOMASTIA
It is natural to have questions about cosmetic surgery. We are committed to helping you understand the surgical considerations taken to plan a male breast reduction. Well-informed patients are better equipped to make decisions about gynecomastia surgery.
Developmental gynecomastia commences concurrently with puberty. The majority of these adolescent cases spontaneously resolve and eventually disappear. When gynecomastia persists into adulthood, cosmetic improvement by male breast reduction can be considered.
Less common causes for male breast enlargement include diseases of the pituitary gland, endocrine dysfunction, medications, tumors, illness, and recreational drug use.
Nonsurgical gynecomastia treatments have little or no effect. Be suspicious of product advertisements and nonscientific articles saying otherwise. The topical application of skin creams is not effective at reducing gynecomastia. Surgical male breast reduction is the only effective solution.
Men with gynecomastia considering male breast reduction should be in good health, have stable body weight, have no serious or active illnesses, no pre-existing medical conditions, and must have realistic outcome expectations. Patients developing gynecomastia from anabolic steroid use must cease and reframe from use in the future.
Gynecomastia surgery is not a treatment for obesity nor a substitute for good nutrition and exercise. Potential patients intending to lose weight should delay their male breast reduction until they have reached a stable body weight. It is important to discuss weight loss plans with your plastic surgeon before surgery.
Despite the swelling associated with surgery, meaningful results are apparent immediately following male breast reduction. In the months following gynecomastia surgery, the edema will resorb and the skin will retract to further accentuate the masculine chest contours gained by male breast reduction.
Gynecomastia refers to male breast enlargement resulting in a feminine chest contour. The tissue composition of the enlarged breast is biologically comprised of fat and mammary gland.
Glandular gynecomastia most often appears as an oval subareolar mass attached to the nipple. The excess breast tissue is firm, inelastic, and does not respond to liposuction. Direct excision techniques are necessary when planning glandular gynecomastia surgery. Anabolic steroid use and innate hormone sensitivity are thought to be potential causes of glandular gynecomastia.
Fatty gynecomastia is principally composed of excess fat. Its causes are more diverse. Hormonal sensitivity, obesity, steroids, and medications all may trigger this condition. The excess fat is diffusely spread throughout the breast and chest. With fatty gynecomastia, the breast is soft, compressible, and blends indistinctly with adjacent normal tissue. Liposuction is especially effective in the treatment of fatty gynecomastia.
Most patients presenting with gynecomastia have an excess of fat and gland. Optimal gynecomastia treatment outcomes are usually achieved with a combination of liposuction to aspirate fat and direct surgical excision to remove the gland.
Mild and moderately severe grades of gynecomastia do not require skin excision and often heal with minimal scars (at access points used for liposuction and direct excision). Liposuction scars are tiny and imperceivable. Direct excision access incisions are strategically positioned around the areola and/or inframammary fold. The resulting scars are short and concealed at the margin of the areola or hidden in the inframammary crease.
Severe forms of gynecomastia with excess skin necessitate skin excision and nipple grafts. Unfortunately, the skin excisions do result in visible scars around the areola and at the inframammary crease.
Gynecomastia surgery results in mild discomfort, swelling, and bruising. These symptoms spontaneously and gradually improve over the weeks following surgery. The expected discomforts respond well to mild analgesics such as Tylenol.
We tailor our physical activity recommendations to every patient’s unique situation. Patients having local anesthesia for minor gynecomastia surgery can often return to their usual routines without disruption. For moderate male breast reduction performed under general anesthesia, we advise a 1-week cessation of work. Return to sports and intense physical activities is usually possible after 3 weeks.
Preparation for Gynecomastia Surgery
- Avoid nonsteroidal anti-inflammatory medications (Aspirin, Advil, etc.)
- Stop smoking, do not use e-cigarettes, avoid nicotine and marijuana
- Do not drink alcohol
- Continue prescription medications (unless advised otherwise)
Day of Surgery
- Stay fasted from midnight prior to surgery (no food, no drinks)
- Be punctual – Arrive on time to the surgery facility
- Wear loose clothing – Avoid the use of cosmetics
- Come accompanied by a responsible person (transportation home)
Advice after Gynecomastia Surgery
- Do not cook, clean, carry weight (groceries or children), or drive
- Take your medications as prescribed
- Notify us promptly of unexpected symptomatology
- Do your best to rest and relax for 2 weeks